BioElectronic-Medicine
“Imagine a day when electrical
impulses are a mainstay of medical treatment.” These
words, by GlaxoSmithKline’s head of bioelectronics R&D
unit Kristoffer Famm, appeared in Nature in 2013, the same
year in which the British company launched a $50 million
initiative to advance neuromodulation research. Although
the phrasing probably sounded farfetched at the time, recent
advancements support the revolutionary potential of so-called
electroceuticals and shed light on the integral role they are
bound to play in the future of medicine. In fact, modulation
of nerve signals to control organ function has been
increasingly recognized as a powerful, new way to treat a wide
range of diseases. The present article will give an overview
of ongoing neuromodulation research and discuss the R&D
tax credit opportunities available to support companies as
they move forward into the era of bioelectronic medicine.
The Research &
Development Tax Credit
Enacted in 1981, the Federal Research and
Development (R&D) Tax Credit allows a credit of up to 13
percent of eligible spending for new and improved products and
processes. Qualified research must meet the following four
criteria:
- New or improved products,
processes, or software
- Technological in nature
- Elimination of uncertainty
- Process of experimentation
Eligible costs include employee wages, cost of supplies, cost
of testing, contract research expenses, and costs associated
with developing a patent. On December 18, 2015 President Obama
signed the bill making the R&D Tax Credit permanent.
Beginning in 2016, the R&D credit can be used to offset
Alternative Minimum tax and startup businesses can utilize the
credit against $250,000 per year in payroll taxes.
Understanding
Electroceuticals
The nervous system is key to the control of
our physiology. Peripheral nerves connect each and every part
of the body to the brain and spinal cord and use patterns of
electric impulses, called action potentials, to establish
communication between them. This complex network plays a
crucial role in the maintenance of physical and mental health.
On the one hand, it continuously monitors the body’s health
status and responds to disease by adjusting organ function to
initiate the healing process. On the other hand, however, it
can be the source of pain, metabolic disorders, and autoimmune
conditions that are caused by disruptions in nerve signaling.
Ongoing bioelectronic research aims to learn the body’s
“electrical
language” and develop advanced
implantable devices capable of harnessing the electrical
patterns sent out by the nervous system in order to control
organ function. The idea is to decipher and modulate neural
signaling to trigger the body’s natural ability to heal
itself. Bioelectronics aim to provide targeted, personalized
treatments that work in a closed-loop; electric activity and
associated physiological parameters are recorded and analyzed
in real time so that neural signaling can be modulated
accordingly. Put simply, bioelectronic devices should be able
to constantly monitor patients and automatically adjust
treatment to their needs.
Though still in its infancy, bioelectronics medicine already
inspires ambitious potential applications. Nerve signals can
target a virtually unlimited number of conditions, serving a
wide variety of purposes, from loosening up airways in asthma
patients to reducing inflammation in Crohn’s disease
sufferers. Also referred to as neuromodulation therapies,
bioelectronics could complement or even replace conventional
drugs, creating a new paradigm in which information contained
in different patterns of electrical impulses – each one with
specific wavelengths and frequencies – become the new
therapeutics, specially designed to influence how an organ or
system functions.
Currently available drug and biologic treatments are often
less than ideal as they commonly involve high development
costs, variable efficacy, and a wide range of side effects.
Despite major advances in the pharmaceutical industry,
treatments remain expensive and costs seem to get higher with
every new development. According to industry group PhRMA, the
average new drug takes a decade and $2.6 billion to reach the
market. Emerging bioelectronics could represent a much
more economical alternative, since implants have long life
spans and could, in theory, be repurposed to treat various
conditions. Additional benefits of neuromodulation include a
considerable reduction in adverse effects, especially when
compared to treatments that saturate the body with extraneous
molecules. Also, lack of treatment compliance, such as
forgetting to take pills, is not an issue in bioelectronic
medicine.
In
June 2014, The National Institutes of Health launched a $248
million Stimulating Peripheral Activity to Relieve Conditions
(SPARC) program, with the objective of advancing the
scientific foundation necessary to the development of more
effective and minimally invasive neuromodulation therapies.
SPARC is organized around four interactive research areas,
namely, 1) Anatomical and Functional Mapping of the
Innervation of Major Internal Organs; 2) Next Generation Tools
and Technologies (to assist in mapping and therapy development
efforts); 3) Use of Existing Market-Approved Technology for
New Market Indications; and 4) Data Coordination, Mapping, and
Modeling Center.
Similarly, the Defense Advanced Research Projects Agency
(DARPA) launched, in August 2014, the Electrical Prescription
(ElectRx) program, aimed at characterizing the anatomy and
physiology of specific neural circuits and identifying their
roles in health and disease. The $79 million initiative also
aims to develop disruptive biological-interface technologies
required to monitor biomarkers and peripheral nerve activity,
as well as deliver therapeutic signals to peripheral nerve
targets.
Challenges Ahead
Even though the idea behind bioelectronics
is somewhat simple, implementation is supremely complex. One
of the first crucial steps is particularly daunting:
understanding the fundamental physiology and biological
mechanisms involved in the neural control of organ function.
In a perhaps oversimplified way, one can say that this task is
two-fold. Firstly, there is a need to untangle the body’s
complex “wiring”. In other words, researchers need to figure
out which neural circuits control which organ functions and
develop detailed, predictive circuit maps. This knowledge of
the nervous system’s functional relationships is imperative
for developing effective, targeted treatment. The second
aspect pertains to the particularities of the “electrical
conversation”. Researchers must identify the precise patterns
and frequencies that affect specific organ functions as well
as the changes caused by disease.
Many innovative efforts currently focus on drawing a map of
neural circuits that can guide future bioelectronic
developments. At MIT, for instance, researchers are using a
technique known as “expansion microscopy”, which amplifies
nervous tissue so that their intricate connections can be
observed at a much higher resolution. This is made possible by
embedding tissue samples with a polymer that swells when
exposed to water.
Another groundbreaking method is optogenetics, which utilizes
an artificial virus to make neurons sensitive to light and
thereby allows researchers to switch them on and
off. Menlo Park, California-based Circuit
Therapeutics has used this approach to develop technology that
excites and inhibit nerve cells. By enabling targeted and
immediate control of neural activity, it allows for the
identification and characterization of individual nerve cells
and circuits involved in normal and pathological conditions.
In
2013, Boehringer Ingelheim and Circuit Therapeutics initiated
a three-year research collaboration to explore neural pathways
in psychiatric disorders. In August 2015, the two companies
announced another partnership aimed at investigating the
neural circuits involved in obesity as a means to develop new
treatments for metabolic diseases. In December of the same
year, Circuit Therapeutics was awarded a $2.7 million contract
under DARPA’s ElectRx program to fund efforts related to
neuropathic pain.
In
addition to the science gap that needs to be filled, the
practical aspects of building reliable, closed-loop
neuromodulation devices are also challenging. Even though
medical applications of electricity are not new – examples
include pacemakers and deep-brain stimulation treatments -
bioelectronics is a significantly more complex enterprise.
Implants must combine small dimensions, as little as a cubic
millimeter, with enough robustness to run powerful
microprocessors. Also, they must be made of stable materials
that do not transform over time and, most importantly, do not
damage delicate nerves. Due to extremely reduced dimensions,
traditional choices, such as metal and plastic, are not
considered ideal, since they can hurt the human tissue.
While possible materials include adhesives and magnets, both
GSK and DARPA are betting on a shape-memory polymer that
becomes flexible when exposed to heat. The idea is to leverage
the sensitivity to high temperatures to shape the implanted
devices, making them “hug” the targeted nerves. Another
promising alternative is the use of electrically conductive
synthetic diamonds, which are sensitive to endogenous
chemicals known as neurotransmitters. Researchers at the Mayo
Clinic in Rochester, Minnesota are experimenting with this
material in the fabrication of deep brain stimulation devices.
They aim to build upon the diamond’s ability to measure
neurochemicals to create closed-loop systems that are capable
to autonomously adjust stimulation frequency and amplitude. If
successful, the same principle could be applied to
bioelectronic devices.
A
final and inescapable challenge is security. Bioelectronics
connects patients’ nervous systems to a network of computers
that act as remote controls to their bodies. In this scenario,
the possibility of malignant hacking becomes a major threat.
R&D efforts focused on overcoming potential
vulnerabilities are key to a widespread adoption of
neuromodulation technology.
An Opportunity for the
Pharma Industry
In August 2013, GSK launched a $50 million
strategic venture capital fund with the objective of having
its first bioelectronics product ready for approval in the
following decade. Since then, the British drugmaker has funded
over 80 external researchers and started a competition with $6
million available to fund teams working on implants.
Bioelectronic medicine represents a major opportunity for GSK
and other pharmaceutical companies that must face an
increasingly aggressive market when long and expensive trials
are not always successful and existing products are bound to
face generic competition at some point. GSK’s innovative move
towards bioelectronics questions the traditional divide
between drug companies and medical device companies and shed
light on a promising way forward for the pharma industry.
According to Bloomberg Businessweek, GSK plans to begin human
trials of neuromodulation therapies for three major chronic
diseases in 2017. While these initial tests will use
third-party devices, the company aims to have its first
implant produced by 2019.
New Google/ GSK Joint Venture
On
August 1st, 2016 Google and GSK announced the creation of a
new bioelectronics joint venture called Galvani
Bioelectronics. GSK teamed up with Google’s holding company,
Alphabet Verily Life Sciences, to create the new joint
venture. The company was named after the late Luigi Aloisio
Galvani, the 18th century Italian pioneer of research into
electricity. The goal is to create and commercialize
bioelectronic medicines through miniature implants that
correct electrical signaling along nerves .
Galvani Bioelectronics
will be based in Stevenage, in the United Kingdom, where GSK’s
main research center resides. The company will begin by
establishing clinical proofs of principle in inflammatory,
metabolic, and hormonal disorders (including type 2 diabetes),
while simultaneously developing miniature implants for use in
patients. Researchers aim to intervene outside the brain and
spinal cord in the peripheral nervous system (PNS). The PNS
plays a role in many chronic diseases such as asthma,
arthritis, and diabetes. It is also responsible for
influencing the performance of organs. It is possible that
peripheral nerve stimulation can help treat brain disease by
reducing the overproduction of inflammatory molecules.
Over a course of seven
years, GSK and Alphabet plan to invest £540 million (which
equals over 720 million U.S. dollars). Galvani is expected to
begin clinical trials on bioelectronic medicines in the next
twelve to eighteen months, aiming to be on the market within
ten years.
A Myriad of
Applications
Theoretically, bioelectronics can be
applied to the treatment of a virtually unlimited number of
conditions. Ongoing research supports this claim, as does the
fast-paced growth in experimental devices and targeted
illnesses. The following sections present some exciting
examples.
I.
Inflammatory Autoimmune Diseases
Founded in 2007, SetPoint Medical is devoted to creating
bioelectronics to treat inflammatory autoimmune diseases, such
as rheumatoid arthritis and Crohn’s Disease. The Valencia,
California-based company aims to supplement the body’s
Inflammatory Reflex, a natural mechanism through which the
nervous system regulates the immune system. Their objective is
to use nerve stimulation to activate this natural pathway,
generating a systemic anti-inflammatory effect.
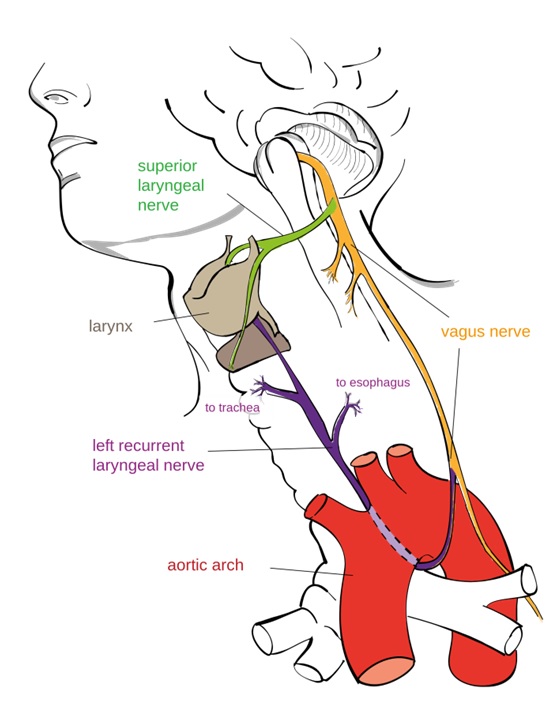
The Inflammatory Reflex was discovered and characterized by
Kevin Tracey, co-founder of SetPoint in the late 90s. Then
researchers at the Feinstein Institute for Medical Research in
Manhasset, New York, Dr. Tracey and his colleagues advocated
the existence of an interface between nerves and immune cells.
Their research demonstrated that “the nervous system was
like a computer terminal through which you could deliver
commands to stop a problem, like acute inflammation, before
it starts, or repair a body after it gets sick. All the
information is coming and going as electrical signals.”
This groundbreaking work pointed to the possibility of
treating different conditions by stimulating the vagus nerve,
which is responsible for conducting impulses to every major
organ in the body. Ultimately, they believed that the delivery
of specific amounts of electricity at precise intervals to the
nervous system could not only reproduce traditional therapies,
but eventually represent cheaper, more effective treatments
alternatives with fewer risks. It was the birth of the
bioelectronics field.
Building upon this
knowledge, SetPoint developed an implantable miniature
neuromodulation device that works as a built-in therapy for
inflammatory autoimmune diseases. Paired with a wireless
charger and iPad control application, the innovative pulse
generator is intended to provide lower cost and improved
safety as compared to drug treatments. The innovative
microregulator is intended to last 10 years thus freeing
patients from repeated injections and pills.
In
November 2012, SetPoint completed a first-in-human open-label
proof-of-concept trial in rheumatoid arthritis patients, which
validated neuromodulation as a potentially revolutionary
therapy for autoimmune inflammatory diseases. In December
2014, the company launched a clinical testing to assess the
safety and efficacy of its bioelectronic therapy to treat
Crohn’s Disease. The ongoing study is being conducted at five
different centers around the globe. In September 2015,
SetPoint raised $15 million to further advance its
anti-inflammatory, neuromodulation platform. Besides GSK, the
list of investors included Covidien Ventures, Boston
Scientific, Morgenthaler Ventures, Foundation Medical
Partners, and Topspin Partners.
II.
Heart Failure and Hypertension
Minneapolis, Minnesota-based CVRx is the creator of the
Barostim Therapy for heart failure and resistant hypertension.
The groundbreaking treatment uses patented technology to
electrically activate the Baroreflex, which is the
physiological mechanism that regulates cardiovascular
function. The activation of this natural pathway reduces
sympathetic activity and increases parasympathetic activity
thus restoring the body’s autonomic balance. In 2015, CVRx
presented positive results from a randomized study in which,
after six months of Barostim Therapy, patient symptoms,
functional capacity, and cardiovascular function were
significantly improved, while heart failure hospitalization
days were reduced.
The company’s Barostim Neo, a minimally-invasive, implantable
neuromodulator, is commercially available in over 20 countries
and under clinical evaluation in the U.S. CVRx recently raised
$46 million, bringing its total equity funding to $237
million, as of June 2016.
III.
Cancer
Research has revealed that the bioelectrical communication
among cells plays a key role in the body’s growth and
development. This leads to believe that changes in the cells’
existing electronic signals can generate new patterns of
growth, a possibility with potentially revolutionary impacts
for cancer patients.
Aiming to verify this assumption, researchers at Tufts
University recently used light to manipulate bioelectric
signals from cancer cells in frogs. Their success suggests
that optogenetics can in fact help disrupt the electrical
communication between cancerous cells and healthy ones,
potentially preventing the appearance of new tumors and even
causing the regression of existing ones.
However, the implementation of such groundbreaking technology
poses major challenges, particularly when it comes to
understanding how voltage exchanges work and what their role
is in controlling chemical signaling among cells. In the words
of senior author Michael Levin, Ph.D. “We need to crack
this bioelectrical code. We really need to figure out how
computations in tissues and decision-making about pattern
and cell behavior and so on are encoded in electrical
signaling. That is sort of the next ten years.”
Characterizing the specific electrical signals associated with
tumor growth can revolutionize cancer treatment and
prevention, allowing for the identification of risks even
before tumors start to grow and ultimately altering the course
of the disease.
IV.
Epilepsy
According to the latest data from Centers for Disease Control
and Prevention, 4.3 million American adults suffer from
epilepsy, a disorder of the brain that causes seizures.
Conventional anti-seizure medication and devices deliver
constant therapy, not considering whether the patient is
actually having a seizure or not. This approach has proven to
have chronic side effects with significant, negative impacts.
Aiming to improve the life of epilepsy patients, Mountain
View, California-based NeuroPace developed the RNS System, an
implantable device designed to prevent seizures at their
source. The innovative solution monitors, detects, and
responds to the brain signals that cause seizures and are thus
automatically activated only when needed. Each device is
tailored to recognize the patient’s specific electrical
patterns so that it can rapidly identify and disrupt abnormal
activity before it leads to seizure symptoms.
V.
Artificial Limbs and Paralysis
In
theory, bionic limbs should work just as real ones. They
should operate on signals sent by the brain, nerves, and
muscles; doing exactly what the patient wants it to. However,
current technology, which traditionally relies on electrodes
placed on the patient’s skin, has encountered some challenges
when it comes to reliably processing the body’s electrical
signals over extended periods of time.
Researchers at Purdue University Center for Implantable
Devices are using bioelectronics to overcome these challenges.
They have developed small, internal electrodes that can be
placed inside the amputee’s remaining muscles. The innovative
electrodes are capable of reading nerve signals more clearly
than traditional ones and can therefore improve the
performance of artificial limbs. Purdue’s groundbreaking
technology was recently licensed by Coapt, a provider of
intuitive control systems for advanced prosthetic arms. The
Chicago, Illinois-based startup describes the technology as
“game-changer” and expects it to give amputees unprecedented
freedom of movement.
Yet another exciting application of bioelectronics is
overcoming paralysis. Researchers at the Feinstein Institute
have recently unveiled an innovative “neural bypass” system,
which consists of an implantable device located in the brain
that records electrical signals generated when patients try to
move their paralyzed limbs. After being decoded by a computer,
the signals are sent out to an electronic sleeve (in the case
of paralyzed hands or arms), which stimulates the muscles,
jolting them into action. In the study, published in May 2016,
a patient with quadriplegia from a spinal injury was able to
perform functional tasks relevant to daily living, which
involved grasping, manipulating, and releasing objects.

Conclusion
Bioelectronics research points to a future in which people
afflicted by disease will not have to take pills and be
exposed to their side effects. Instead, by leveraging our
existing nerve circuits, technology will enable the body to
heal itself.
The many advances reported in this article are just a glimpse
into the revolutionary potential of electroceuticals. R&D
tax credits are available to support innovative companies
dedicated to overcoming outstanding challenges and realizing
the extraordinary potential of neuromodulation therapies.